Introduction
Cancer remains one of the most pressing global health challenges of the 21st century, accounting for millions of deaths annually and imposing a tremendous emotional and economic burden on societies worldwide[1]. Despite advances in diagnostic techniques and therapeutic interventions, conventional treatment strategies such as chemotherapy, radiation therapy, and surgical resection are frequently associated with significant limitations. These methods, while effective in many early-stage or localized cancers, often lack the precision to selectively target malignant cells without affecting normal, healthy tissues. This non-specificity not only leads to collateral tissue damage but also contributes to severe systemic side effects, therapy resistance, and tumor relapse. Additionally, cancer is not a single, uniform disease; it represents a highly heterogenous group of disorders characterized by complex molecular alterations, including genetic mutations, epigenetic dysregulation, uncontrolled cellular proliferation, angiogenesis, and metastatic potential. The dynamic and multifactorial nature of cancer necessitates the development of advanced, multifaceted therapeutic modalities.
What is Nanotheranostics?
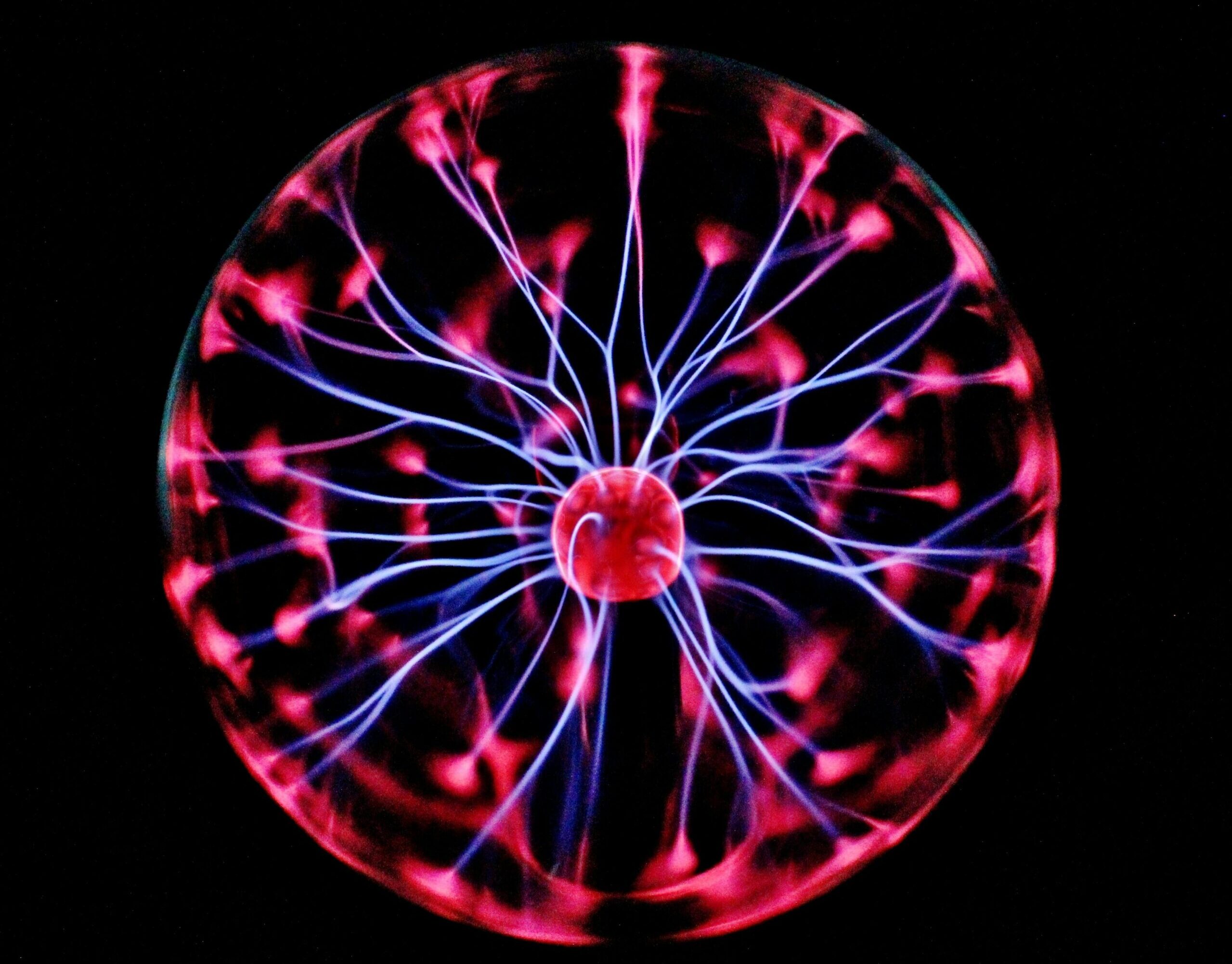
In response to these challenges, nanotheranostics has emerged as a transformative approach in cancer research and clinical oncology. The term “nanotheranostics” refers to the integration of diagnostic and therapeutic functionalities into a single nanostructured systemm typically ranging from 1 to 100 nm in size[2]. These nanoscale platforms-often constructed using materials such as liposomes, dendrimers, gold nanoparticles, or polymeric nanocarriers are engineered to navigate the biological milieu with high specificity. Functionalization with targeting ligands (e.g., antibodies, peptides, or aptamers) allows these nanostuctures to recognize and bind tumor-specific biomarkers or receptors, enabling site-specific drug delivery while simultaneously facilitating real-time imaging through techniques such as MRI, fluorescence, PET, or CT. This dual capability supports not only accurate localization of tumors but also spatiotemporal monitoring of therapeutic efficacy, thereby reducing guesswork in treatment planning[3]. Further amplifying the efficacy of nanotheranostic systems is the incorporation of plant-derived phytochemicals, which are bioactive secondary metabolites with demonstrated anticancer properties. Compounds such as flavonoids, alkaloids, terpenoids, and saponins have shown ability to induce apoptosis, inhibit angiogenesis, modulate immune responses, and suppress tumor metastasis. However, many phytochemicals suffer from poor solubility, rapid metabolic degradation, and low bioavailability when administered in free form. Nanoformulations can overcome these pharmacokinetic limitations by encapsulating phytochemicals within biocompatible carriers, protecting them from enzymatic breakdown and enhancing their accumulation at the tumor site via the enhanced permeability and retention (EPR) effect.
Role of Artificial Intelligence and Machine Learning
Navigating the intricacies of cancer biology requires more than just effective therapeutic agents as it demands intelligent, adaptive systems capable of interpreting vast and complex datasets. This is where Artificial Intelligence(AI) and Machine learning(ML) are playing a transformative role. These technologies are particularly well-suited for oncology, a field characterized by heterrogeneity in tumor biology, patient response variability,and massive multidimensional data stemming from genomics, proteomics, metabolomics, imaging, and electronic health records(EHRs). AI algorithms ranging from decision trees and support vector machines to advanced deep learning models can detect hidden patterns and correlations within these datasets that are often imperceptible to human researchers. In the context of nanotheranostics, AI serves multiple critical functions. Firstly, it can identify patient-specific risk profiles by analyzing genetic mutations, gene expression patterns, and clinical biomarkers, enabling early and accurate cancer diagnosis. Secondly, AI models are capable of predicting tumor progression and drug response by integrating dynamic biological signals with prior treatment outcomes, thus informing real-time therapeutic decisions. Thirdly, AI facilitates the rational design of personalized treatment regimens, ensuring that the selected drugs, dosages, and delivery methods are optimized for the individual’s tumor microenvironment. Furthermore, AI enhances the formulation and functionalization of nanoparticles, predicting how variables such as size, charge, and surface chemistry affect biodistribution, cellular uptake, and immunogenicity. This streamlines the development of nanocarriers for both diagnostic imaging agents and therapeutic payloads, including plant-derived phytochemicals.[4]
Relationship between AI/ML and Nanotheranostics
The workflow of a typical AI-guided, phytochemical-based nanotheranostic system exemplifies the power of this interdisciplinary synergy. It begins with data analysis, where AI algorithms ingest and interpret vast clinical. molecular, and imaging datasets to construct a patient-specific treatment strategy. Next, nanoparticle formulation is executed, often involving the encapsulation or conjugation of selected phytochemicals which are known for their anticancer, anti-inflammatory, and antioxidant properties into biocompatible nanocarriers such as liposomes, dendrimers, or gold nanoparticles. These nanoparticles are then subjected to targeted delivery, a process enabled by surface functionalization with ligands (e.g., antibodies, aptamers, or peptides) that bind specifically to overexpressed receptors on cancer cells. This selective targeting ensures high therapeutic efficacy while minimizing off-target effects and damage to healthy tissues. Simultaneously, real-time imaging modalities are integrated into the same nanoplatform enable clinicians to visualize the biodistribution and accumulation of therapeutic agents at the tumor site. Techniques such as fluorescence imaging, Magentic Resonance Imaging(MRI), and Positron Emission Tomograpgy(PET) allow for monitoring drug release, tumor shrinkage, and treatment responsiveness with high spatial and temporal resolution. This “diagnose and treat” model, facilitated by AI and nanotechnology, represents a significant leap from traditional therapeutic approaches that separate diagnostics and intervention into distinct processes. By unifying these elements into a single, dynamic workflow, nanotheranostics dramatically enhances the precision, efficiency, and adaptability of cancer care.
Future scope, Challenges and Conclusion
While nanotheranostics presents a gorundbreaking approach to cancer care, several challenges must be addressed before it can become a standard clinical tool. Key concerns include the biocompability and long-term safety of nanomaterials, as some nanoparticles may accumulate in tissues or elicit immune responses. The scalability and reproducibility of nanoparticle production also remain technical bottlenecks, especially when transitioning from laboratory synthesis to industrial-scale manufacturing. Additionally, regulatory uncertainties surounding the approval of phytochemical-based therapies and ethical issues related to AI, such as algorithm trnasparency, data privacy, and clinical accountability which further complicates integration into healthcare systems. Despite these obstacles, rapid progress in bioinformatics, computational biology, and nanomaterial engineering is steadily overcoming these limitations and moving the field toward clinical readiness. At its core, nanotheranostics represents a fusion of plant-based therapeutics, intelligent nanocarriers, and AI-powered analytics, offering a highly personalized and minimally invasive strategy for cancer management. This integrated system enables targeted drug delivery, real-time imaging, and adaptive treatment planning based on each patient’s unique molecular profile. By minimizing off-target effects and enhancing therapeutic precision, nanotheranostics holds the potential to significantly improve treatment outcomes. As interdisciplinary research continuesto evolve, this approach is poised to transform cancer therapy into a more efficient, patient-centric, and data-driven discipline, marking a major leap toward the future of personalized medicine.
References:
- Global Burden of Disease Cancer Collaboration. (2015). The global burden of cancer 2013. JAMA oncology, 1(4), 505.
- Singh, V. (2024). Theranostics: Integrated Diagnostics and Therapy Using Nanomedicine. In Nanomedicine (pp. 505-530). Springer, Cham.
- Bai, J. W., Qiu, S. Q., & Zhang, G. J. (2023). Molecular and functional imaging in cancer-targeted therapy: current applications and future directions. Signal Transduction and Targeted Therapy, 8(1), 89.
- Chavda, V. P., Nalla, L. V., Balar, P., Bezbaruah, R., Apostolopoulos, V., Singla, R. K., … & Uversky, V. N. (2023). Advanced phytochemical-based nanocarrier systems for the treatment of breast cancer. Cancers, 15(4), 1023.