
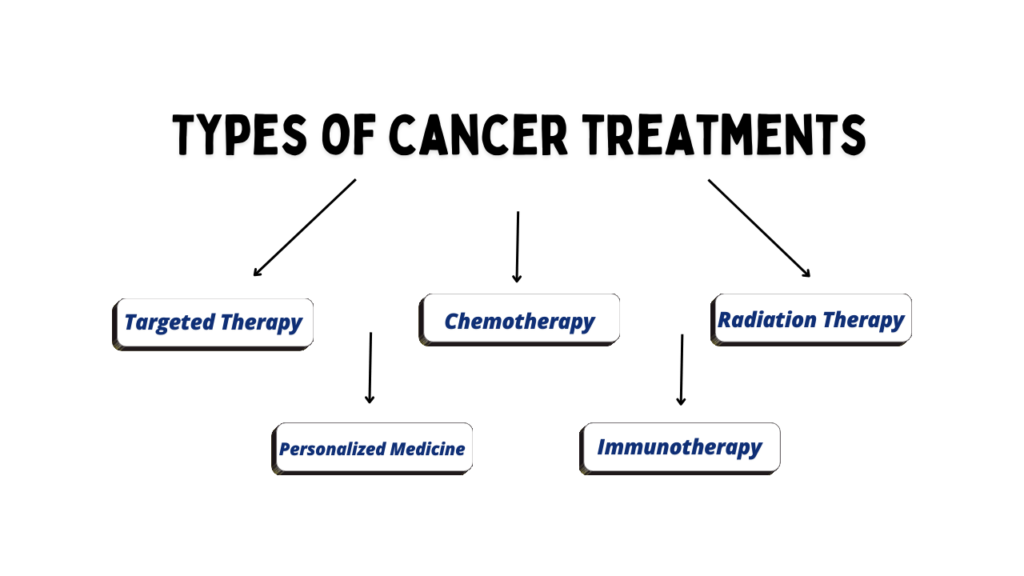
Cancer is one of the principal causes of deaths worldwide, although the development of treatments has grown significantly over the last few decades. While in the past, patients could only choose between surgery, chemotherapy, or radiation, currently, we observe an era with increasingly sophisticated treatments, including targeted therapies, immunotherapies, and even personalized treatments, based on the genetic makeup of tumours. Let us explore the evolution of cancer treatments, their mechanisms of action, their applications, and their limitations, with a focus on the journey from traditional chemotherapy to cutting-edge immunotherapies.
Chemotherapy: The Pillar of Cancer Treatment
Chemotherapy is often the first line of defense against many types of cancer. Since its introduction in the 1940s, it has been a cornerstone of cancer treatment, albeit with significant limitations. It works by targeting rapidly dividing cells, a hallmark of cancerous growth. Cancer cells divide much more rapidly than normal cells, so chemotherapy drugs aim to disrupt the cell cycle, preventing these cells from multiplying. Most chemotherapy agents interfere with DNA replication or the mitotic spindle, causing cell death (apoptosis) in dividing cells. The main categories of chemotherapy drugs include alkylating agents, antimetabolites, and mitotic inhibitors.
Now, every treatment or solution, no matter how effective, comes with its own set of limitations and potential side effects. Similarly, chemotherapy may be effective at killing cancer cells, but it also kills other healthy cells. The cells most affected are those that divide the fastest, like those in the bone marrow, hair follicles, and the digestive tract. This leads to common side effects such as Myelosuppression (Reduced production of blood cells, causing anaemia, a higher risk of infections, and bleeding) Alopecia (Loss of hair caused by damage to hair follicle cells), Gastrointestinal toxicity etc.
Chemotherapy fails to address most cancers. Some cancer types get resistant after years of use due to how fast cancer cells learn to be mutated and become evasive from chemotherapy drugs.
Radiation Therapy: Targeting Tumours with High-Energy Rays
Radiotherapy evolved as a complementary approach to chemotherapy, offering a more targeted method of cancer treatment by using high-energy radiation to specifically target tumours while minimizing systemic exposure. Radiation therapy makes use of the high-energy radiations that come in the form of X-rays or protons to kill the cancer cells. Unlike chemotherapy, which has systemic effects, the radiation tends to be localized, targeting the specific area where the tumour is situated. Radiation therapy has its mechanism of action at inducing the cancer cells to damage their DNA, either directly on the DNA itself or indirectly by providing free radicals that further lead to DNA damage. At a certain level of damage, the cells are unable to repair themselves; thus, cell death results.
Radiotherapy can be classified into different types, mainly EBRT (involves directing the beam of radiation externally from the outside of the body to hit the tumour through a machine), Brachytherapy (radioactive material is placed within or very close to the tumour) and Systemic Radiation Therapy (where radioactive drugs are introduced via the bloodstream with the aim of eradicating spread cancers throughout the body)
Although radiation may be very effective in shrinking or eliminating localized tumours, it can also damage healthy tissues around the tumour. There may be side effects like fatigue, skin reactions, gastrointestinal issues, and long-term risks such as secondary cancers in irradiated areas.
Surgery: The Oldest and Most Direct Approach
Surgery is a key treatment for localized solid tumours, particularly when the cancer has not spread. It involves the removal of the tumour or affected organ, with the extent of the surgery varying from tumour resection to full organ removal, such as in a mastectomy. However, surgery is typically effective only for non-metastasized cancer, and in cases where the cancer has spread, it may be less effective, though still offering palliative benefits. Additionally, surgical risks include infection, bleeding, and potential damage to surrounding tissues.
Targeted Therapy: Precision Treatment for Cancer
Targeted therapy is a more modern approach to the treatment of cancer, based on specific molecular alterations within cancer cells. Unlike chemotherapy, which kills cells that divide quickly, targeted therapy aims to inhibit the molecular signals that enable cancer cells to grow and multiply.
Targeted therapy drugs are designed to interfere with specific molecules involved in cancer growth, progression, and spread. These include blocking cell surface receptors that many cancers rely on for growth signals, such as the HER2 receptor in HER2-positive breast cancer, which is targeted by trastuzumab (Herceptin). They also target intracellular signaling pathways, like the EGFR mutation in non-small cell lung cancer, inhibited by drugs such as erlotinib or gefitinib. Additionally, angiogenesis inhibitors like bevacizumab (Avastin) block the formation of new blood vessels that tumours need to grow, helping to slow cancer progression.
Though targeted therapies are typically more specific and less toxic than chemotherapy, they also have their limits. Some cancers will develop resistance to targeted drugs, especially when the genetic mutation or molecular target shifts over time. In addition, targeted therapies typically work well in cancers only bearing specific genetic markers, so its use may not be generalized.
Immunotherapy: The Potential of Immunity
Immunotherapy represents a groundbreaking shift in cancer treatment. Rather than attacking the cancer cells directly, immunotherapy works by stimulating the body’s immune system to recognize and fight cancer. This approach has garnered significant attention for its success in treating cancers that were previously considered difficult to treat, such as melanoma and certain types of lung cancer.
It includes a range of treatments; each designed to boost or modulate the immune system’s ability to target and destroy cancer cells. Key categories of immunotherapy include:
- Checkpoint Inhibitors: These drugs block proteins that inhibit immune cells from attacking cancer cells. For example, PD-1 inhibitors like pembrolizumab (Keytruda) and nivolumab (OPDIVO) target the PD-1 receptor, which cancer cells exploit to evade immune detection.
- Monoclonal Antibodies: These antibodies bind to specific markers on cancer cells, prompting the immune system to attack the cancer. Examples include rituximab for lymphoma and trastuzumab for HER2-positive breast cancer.
- CAR T-Cell Therapy: This treatment involves collecting a patient’s T cells, modifying them to better recognize and target cancer cells, and then reintroducing them into the patient. It has shown promising results in treating hematologic cancers like leukemia and lymphoma.
- Cancer Vaccines: Vaccines such as the HPV vaccine help prevent certain types of cancer, while other vaccines are under development to stimulate the immune system to identify and target cancer-specific antigens.
Immunotherapy has demonstrated incredible efficacy in the treatment of certain cancers previously considered to be untreatable. Most notably, checkpoint inhibitors have produced long-term remission in a small subset of patients with advanced melanoma and lung cancer. But not all patients respond to immunotherapy, and some develop autoimmune reactions where the immune system attacks healthy tissues.
Personalized Medicine: Tailoring Treatments to the Individual
Perhaps one of the most exciting concepts in cancer treatment is that of personalized medicines. It uses the genetic and molecular profile of a patient’s cancer to design the most effective treatment regimen. Doctors use genomic profiling to identify mutations and molecular alterations unique to the patient’s tumour, thereby selecting therapies most likely to be effective.
Personalized medicines sometimes employ NGS or other forms of molecular testing to examine the tumour’s genetic signature. Information gleaned can reveal mutations in specific genes (e.g., EGFR, BRAF, or PIK3CA), leading the physician to guide treatment with specific targeted therapies, immunotherapies, or clinical trials specifically targeting these alterations.
The complexity and heterogeneity of the cancer make up the challenge with personalized medicine. Most cancers are non-mutant, and mutation occurs in progression that eventually produces resistance to drugs. Furthermore, genomic testing is costly, which means targeted therapies will not reach some patients in need.
CONCLUSION
The entire landscape of cancer treatment is changing rapidly from traditional chemotherapy and radiation to innovative therapies like immunotherapy and personalized medicine. Despite the fact that chemotherapy and radiation are still integral in cancer treatment, the trend to a more focused, accurate approach ultimately promises better results with fewer side effects. Immunotherapy alone has become the savior in many previously intractable cancers, but challenges persist in managing patient response and adverse effects.
As the research advances, combination of different modalities, such as immunotherapy with chemotherapy, radiation, or targeted therapies, may have the best opportunity to enhance survival chances and quality of life for patients diagnosed with cancer. The future of cancer treatment is likely to be tailored to individualized gene expression profiles of the type of cancer in each patient.
References
“Cancer: Principles & Practice of Oncology” by Vincent T. DeVita, Theodore S. Lawrence, and Steven A. Rosenberg – This textbook is a comprehensive resource on cancer treatment, including radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
“Abeloff’s Clinical Oncology” edited by John E. Niederhuber, James O. Armitage, and Michael B. Kastan – A detailed resource on cancer biology, treatment strategies, and therapeutic approaches including surgery, chemotherapy, and advanced therapies.
“Basic Clinical Oncology” by John F. Griffin – A book that covers the fundamentals of cancer treatment modalities, including surgery and radiotherapy, in an accessible format for medical professionals.
“Principles of Cancer Biotherapy” by Raymond L. Erikson – A more specific resource for understanding cancer therapies such as immunotherapy and targeted therapies.
“Molecular Biology of Cancer: Mechanisms, Targets, and Therapeutics” by Stella Pelengaris and Michael Khan – A useful reference for the molecular mechanisms of cancer treatment, with a focus on targeted therapies and genetic profiling.

That was a good read.
Sending love and support to all those affected by cancer. Thank you for sharing this important information and raising awareness about cancer. My heart goes out to everyone fighting this battle.
It was a good read